U.S. health officials are raising alarms about the potential dangers associated with a specific opioid-related ingredient, 7-hydroxymitragynine (7-OH), which is increasingly found in energy drinks, gummies, and dietary supplements sold at gas stations and convenience stores. In response to these concerns, health authorities are recommending a nationwide ban on this substance.
7-hydroxymitragynine is a potent chemical derived from kratom, a plant native to Southeast Asia. This plant has gained traction in the U.S. as an unapproved remedy for various conditions, including pain, anxiety, and dependence on drugs. Recently, dietary supplement companies promoting kratom have called on the Food and Drug Administration (FDA) to take action against products containing 7-OH, labeling it as a dangerously concentrated and synthetic version of the natural ingredient.
According to a statement released by the U.S. Department of Health and Human Services, the FDA’s actions are not aimed at regulating natural kratom leaf products. Instead, the agency is focused on educating the public about the risks associated with 7-OH and distinguishing it from the kratom plant itself. Regulators have suggested that 7-OH be classified under the federal government’s most restrictive list of illegal drugs, which includes substances like LSD and heroin.
FDA Commissioner Marty Makary highlighted the seriousness of the issue, stating, “7-OH is an opioid that can be more potent than morphine.” He emphasized the need for regulation and public education to avert another wave of the ongoing opioid epidemic that has devastated many communities across the nation.
The Drug Enforcement Administration (DEA) will review the FDA’s recommendations, as it is responsible for establishing federal regulations for high-risk drugs, including both prescription medications and illicit substances. However, a federal ban will not take effect until new rules governing 7-OH have been drafted and finalized.
For nearly a decade, federal regulators have been scrutinizing kratom due to reports of addiction, injuries, and overdoses linked to its use. Despite these concerns, users and distributors have consistently opposed regulatory efforts, arguing that kratom may serve as a safer alternative to traditional opioid painkillers, which have contributed significantly to the current drug addiction crisis.
Last month, the FDA issued warning letters to seven companies marketing drinks, gummies, and powders infused with 7-OH. These products were cited for violating FDA regulations, as they had not undergone safety evaluations and, in some instances, claimed to treat various medical conditions, including pain, arthritis, and anxiety.
Supplement executives, like Ryan Niddel of Diversified Botanics, praised the FDA’s proactive stance, stating that it demonstrated the necessary regulatory excellence to protect consumers. Conversely, the American Kratom Association has been lobbying against stricter regulations, advocating for legislation that would prevent the FDA from regulating kratom more stringently than food and dietary supplements.
In 2016, the federal government nearly imposed a ban on kratom, with the DEA planning to classify it as a Schedule I substance. However, the initiative was halted following a significant public outcry, including a letter signed by over 60 members of Congress. The FDA subsequently began a comprehensive study of kratom, concluding in 2018 that it comprises many of the same chemicals found in opioids, which are known for their addictive nature.
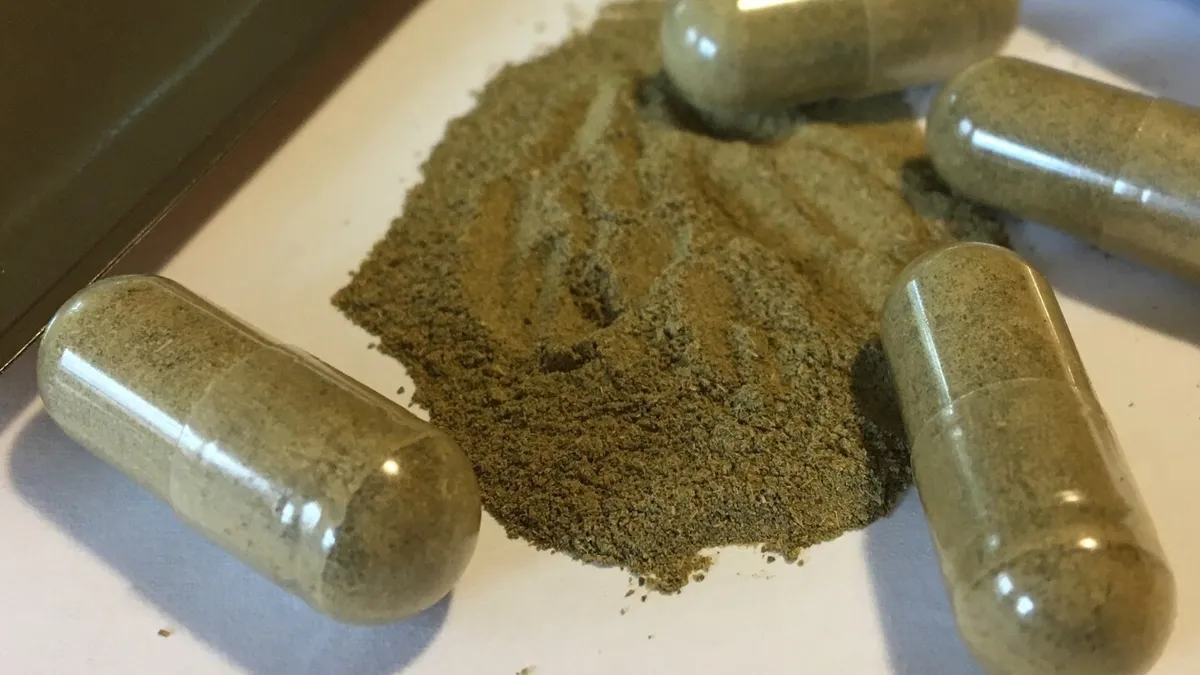
Since that time, the FDA has continued to issue warnings regarding the risks of kratom supplements, which are primarily sold in capsule or powder forms. In recent months, the agency has also targeted other unapproved substances marketed as supplements or energy drinks, such as the antidepressant tianeptine, which has been colloquially referred to as “gas station heroin.” While some states have restricted these substances, they remain unscheduled at the federal level.
The Associated Press Health and Science Department acknowledges support from the Howard Hughes Medical Institute’s Department of Science Education and the Robert Wood Johnson Foundation. However, the AP is solely responsible for the content of this article.