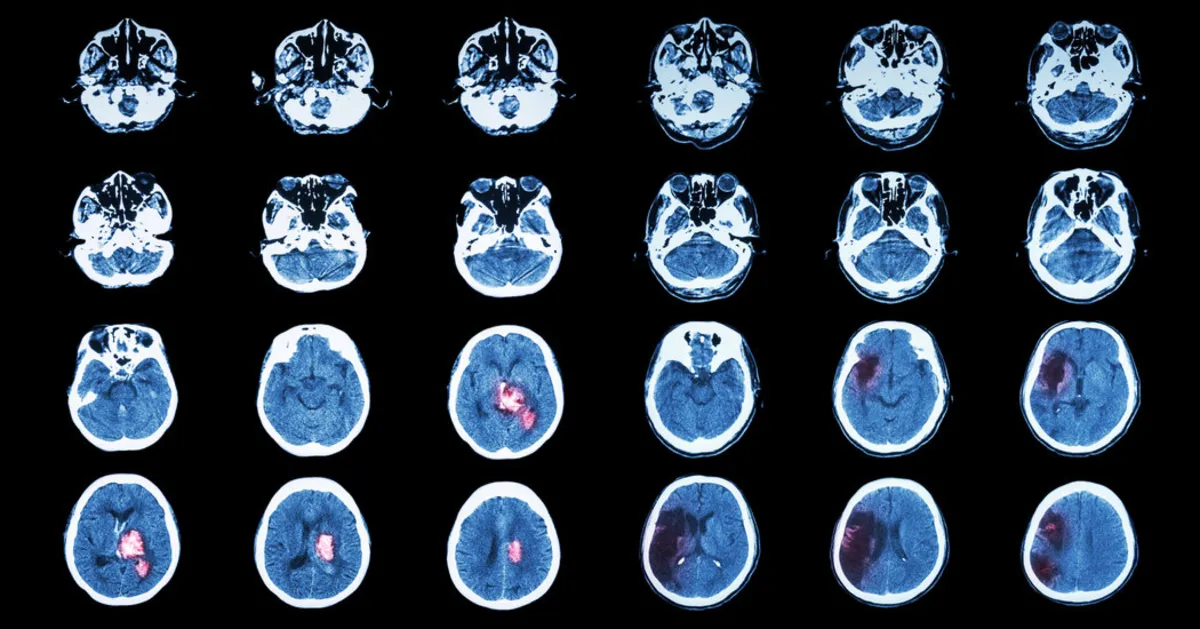
For the past 15 years, Dr. Sean Dukelow has been a dedicated physician treating stroke patients at Foothills Hospital in Calgary, Canada. Throughout his career, he has primarily relied on a singular approach: neurorehabilitation. This method emphasizes the importance of repeating specific actions in therapies such as speech therapy, physical therapy, and occupational therapy. This repetition is crucial as it taps into the brain’s natural plasticity, fostering neuron growth and creating new neural connections.
Dr. Dukelow emphasizes the necessity of this repetition by stating, “There’s going to be a lot of repetition.” However, he also points out a significant gap in available therapies that can enhance long-term recovery. Current options are primarily invasive implants that stimulate the vagus nerve or the spinal cord, leaving patients with limited choices for non-invasive recovery methods. Now, neurologists are racing against time to discover groundbreaking substances or devices that can provide a much-needed “turbo boost” to facilitate brain recovery.
According to Dr. Dukelow, this turbo boost could be critical for patients striving to regain basic functions. He notes, “That turbo boost may be the difference between you walking again, talking again, being able to get home, versus having to go to a nursing home.” As the search for effective treatments continues, several promising candidates are emerging, including transcranial magnetic stimulation (TMS), antidepressant medications, and psychedelics. These therapies are primarily known for their efficacy in treating mental health conditions such as depression, post-traumatic stress disorder, and obsessive-compulsive disorder.
In the realm of psychiatry, these innovative methods are believed to interact with the brain circuits responsible for memory and learning, the same circuits that may facilitate stroke recovery. The goal is to not only alter detrimental thought patterns but also to assist the brain in discovering alternative pathways to perform functions like walking, speaking, and remembering, effectively bypassing damaged neurons.
One of the most discussed treatments in the context of stroke recovery is transcranial magnetic stimulation. Unlike its predecessor, electroconvulsive therapy, which has garnered a negative reputation, TMS is generally painless and does not involve seizures. The process utilizes coils that are placed around the scalp to deliver brief magnetic pulses comparable in strength to those produced by an M.R.I. machine. Dr. Mark George, a pioneering neurologist at the Medical University of South Carolina, describes TMS as a “clever trick” that stimulates brain circuits by penetrating the skull without invasive procedures.
While TMS has shown promise in treating conditions such as obsessive-compulsive disorder, migraines, and aiding in smoking cessation, its effectiveness for stroke recovery remains a subject of debate among experts. Clinical trials have been limited in size and have produced mixed outcomes. However, in April 2025, Dr. Dukelow released results from a small trial indicating that TMS, when combined with intensive speech therapy, could significantly improve fluency in stroke survivors even more than six months post-stroke. Notably, one participant was able to relearn two of the four languages she had lost due to the stroke.
In conclusion, as research continues to evolve, the potential for innovative treatments like TMS and other neurorehabilitation strategies may redefine the landscape of stroke recovery. While traditional therapies remain integral to rehabilitation, the pursuit of new methods offers hope for enhanced recovery outcomes and improved quality of life for stroke survivors.