Menopause can usher in a host of disruptive symptoms, including hot flashes, night sweats, and sleep problems. For many women experiencing these challenges, hormone therapy offers a potential solution. However, the decision to pursue this treatment often comes with questions and concerns, primarily due to its complex history and the ongoing debate surrounding its safety and effectiveness.
The landscape of hormone therapy has evolved significantly over the years. Once routinely prescribed, its use faced scrutiny after a 2002 study raised alarms about increased risks of breast cancer and blood clots. Although subsequent research has indicated that the benefits of modern hormone therapies may outweigh the risks for many women, the lingering concerns have left many feeling confused and apprehensive. “There is still a lot of confusion and a lot of fear,” noted Grayson Leverenz, a 50-year-old from Durham, North Carolina, who ultimately decided to pursue hormone therapy and has found relief.
Recent discussions, including a panel convened by the Food and Drug Administration (FDA), have suggested that health warnings associated with some hormone therapy formulations may be outdated. Experts emphasize that while hormone therapy can be a beneficial option for numerous menopausal women, it's essential to understand the nuanced reality of these treatments and make informed decisions. "Hormone therapy is a great option for many, but not all, menopausal women," experts advise.
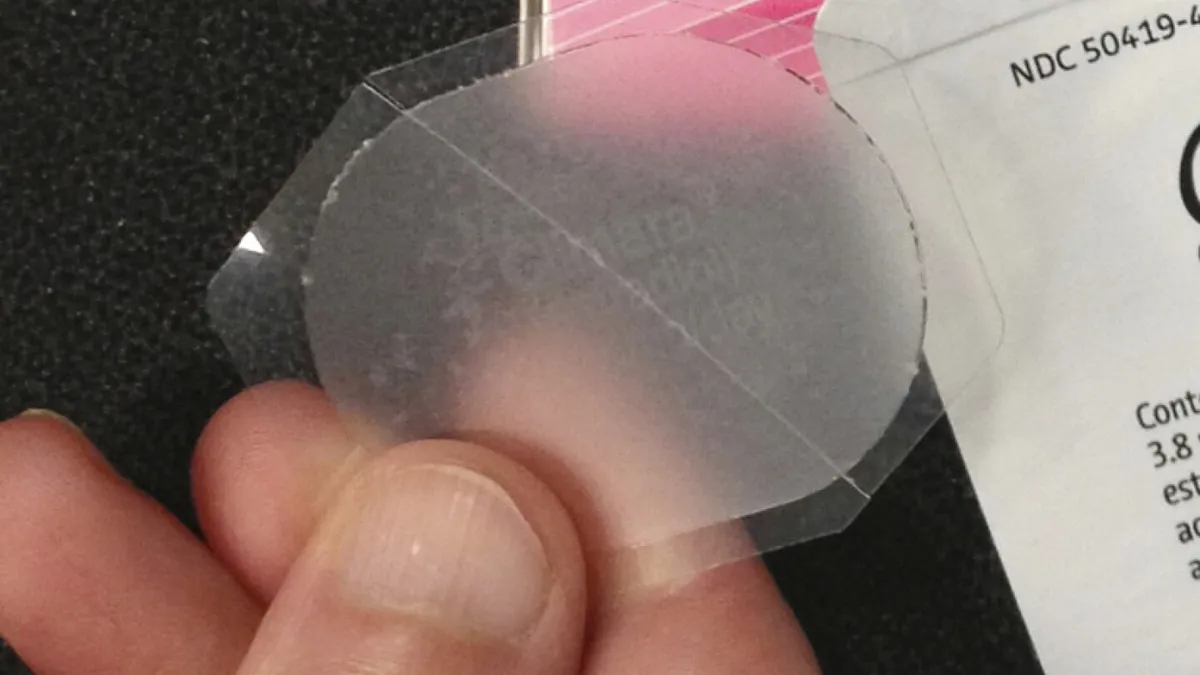
Hormone therapy effectively addresses symptoms that arise as menstruation ceases, leading to significant drops in estrogen and progesterone levels. One common form is low-dose vaginal estrogen therapy, which minimizes systemic circulation and associated risks, making it a suitable choice for women primarily dealing with vaginal dryness. Conversely, systemic hormone therapy involves the use of pills, patches, sprays, gels, or vaginal rings that deliver higher doses of hormones directly into the bloodstream to alleviate symptoms like hot flashes.
Jennifer Zwink, a nurse from Castle Rock, Colorado, shared her positive experience with an estrogen patch in combination with an IUD for progesterone. “It’s not like a 100% magic wand,” she remarked, “but it definitely has made a significant difference,” highlighting the potential improvements in sleep, hot flashes, and joint pain.
The Menopause Society indicates that initiating hormone therapy within ten years of menopause may lower the risk of cardiovascular disease, reduce the likelihood of developing Type 2 diabetes, and help maintain bone density for longer periods. “They might have a drop in their bone density at age 60 instead of at age 50,” explained Dr. MargEva Morris Cole, an OB-GYN with Duke University.
Despite the potential benefits, many women remain hesitant to start hormone therapy due to concerns about associated risks. Leverenz, who was initially apprehensive, ultimately decided to proceed with a combination of hormone medications, resulting in significant improvements in her quality of life. Doctors note that while estrogen therapy can be safely used for up to seven years, and estrogen-progestogen therapy for three to five years, the associated risks must be carefully considered. These include increased chances of stroke and blood clots, particularly with oral forms of hormone therapy.
Healthcare professionals are currently divided on whether to modify the "black box" warnings that accompany some hormone treatments. These warnings highlight the elevated risks of stroke, blood clots, and cognitive issues among women using these medications. A letter signed by 76 doctors and researchers has urged caution, arguing that altering warning labels without thorough scientific evaluation could jeopardize patient safety.
In the midst of this debate, doctors emphasize the importance of discerning fact from misinformation, particularly claims circulating on social media. Dr. Duke's Cole cautioned against the notion that hormone therapy guarantees a longer and healthier life, stating, “I don’t want the pendulum to go so far that people feel that it is promising health for the next 30 to 40 years.”
For women seeking alternatives to hormone therapy, new options are emerging. One such treatment is fezolinetant, marketed as Veozah, which targets hot flashes and night sweats without hormones. Additionally, low-dose gabapentin, typically used as an anti-epileptic medication, can also help alleviate hot flashes, while moisturizers can effectively address vaginal dryness. Regular exercise and a balanced diet are also recommended for managing menopausal symptoms.
Experts caution against the rapidly growing market of supplements claiming to be ultimate solutions for menopause. “Everybody is in on the menopause gold rush,” Dr. Santoro stated, urging women to remain skeptical of products that appear too good to be true.
In conclusion, while hormone therapy presents an effective option for many women experiencing menopause, understanding the associated risks and benefits is crucial for making informed decisions. As more information becomes available, women are encouraged to consult with their healthcare providers to determine the best course of action tailored to their individual needs.