In recent weeks, the abrupt changes made by federal health officials regarding COVID-19 vaccine recommendations for pregnant women have led to widespread confusion and uncertainty. Reports have emerged of patients being turned away when attempting to get vaccinated, prompting 30 health and medical organizations to advocate for continued access and insurance coverage for these vital vaccines.
In an open letter, prominent organizations, including major professional groups for obstetricians, primary care providers, pediatricians, pharmacists, and nurses, expressed their profound concern regarding the new policy from the Department of Health and Human Services (HHS). “We are deeply concerned about the recently adopted HHS policy to no longer recommend COVID-19 vaccination during pregnancy,” the letter stated. It emphasized the critical need for pregnant women to maintain access to this prevention tool to safeguard themselves and their vulnerable infants, who are not yet eligible for vaccination.
The letter urges “payers and insurers to continue making the COVID-19 vaccine available to pregnant people without undue utilization management or cost-sharing requirements.” This plea comes even as the vaccine has been removed from the list of recommended vaccines by the Centers for Disease Control and Prevention (CDC). Pregnant women infected with COVID-19 face significantly higher risks, including ICU admission, ventilator use, and even mortality.
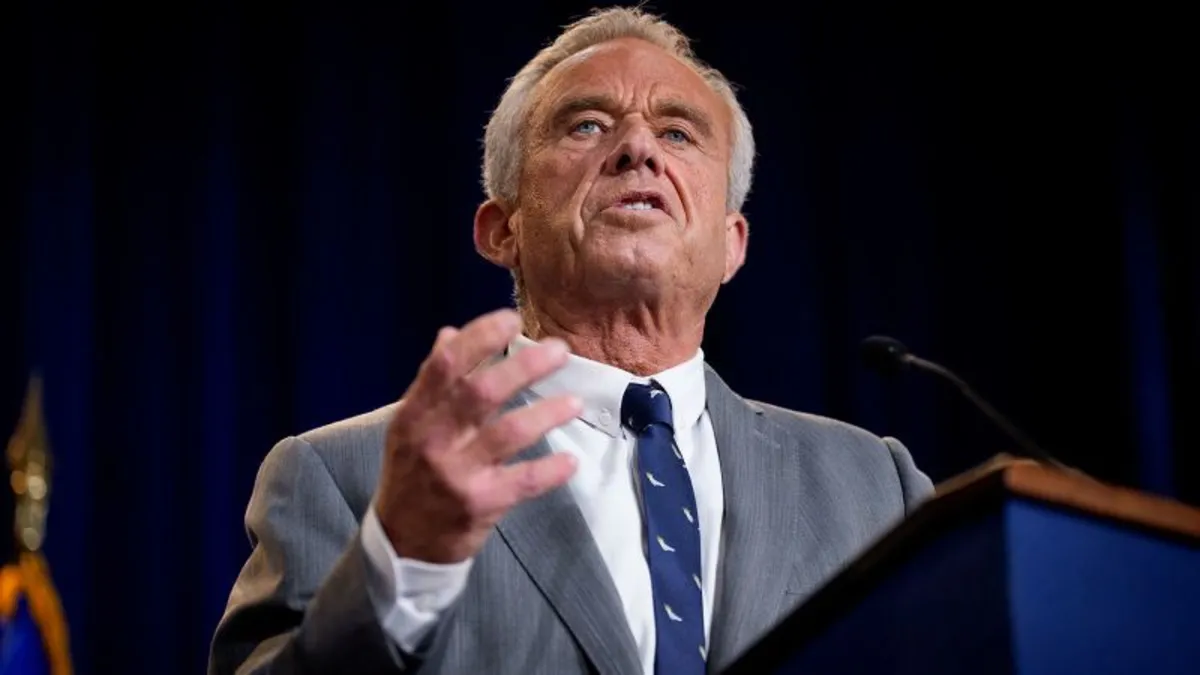
The letter highlights the increased risks of complications such as cesarean birth, preeclampsia, eclampsia, and blood clots for pregnant women. Infants born to mothers who contracted COVID-19 also encounter heightened risks. The clarion call for action from these organizations follows the unexpected announcement by HHS Secretary Robert F. Kennedy Jr., who declared that the COVID-19 vaccine, proven safe and effective during pregnancy, would no longer be recommended.
Additionally, leaders from the U.S. Food and Drug Administration (FDA) have introduced a new framework for the approval process of COVID-19 vaccines, which may limit availability primarily to older adults and those at higher risk of severe illness. Experts fear that these changes could create new barriers for those seeking vaccinations, resulting in confusion about eligibility and potential increases in out-of-pocket costs if insurance coverage is revoked.
The American Pharmacists Association has documented instances of patients being denied COVID-19 vaccines. For example, Leigh Haldeman, a 33-year-old nurse at Harborview Medical Center in Seattle who is pregnant, attempted to get vaccinated but was turned away twice. “Because of some complications I had during my first pregnancy, getting the vaccine now and getting that extra boost of immunity would be definitely important for me,” Haldeman told CNN. Despite having an appointment, she was informed by two different pharmacies that the vaccine was not recommended for pregnant women under the new guidelines.
Despite the shift in recommendations from HHS, many doctors continue to advocate strongly for COVID-19 vaccination during pregnancy. The American College of Obstetricians and Gynecologists reaffirmed that the science has not changed, stating, “It is very clear that COVID-19 infection during pregnancy can be catastrophic and lead to major disability.” They emphasize that vaccination can protect both mothers and their infants.
Haldeman's experience reflects the frustrations many face in navigating the current landscape of COVID-19 vaccination. After being told at a Walgreens that she could not receive the vaccine, she reached out to her obstetrician, who prescribed the vaccine for her. However, when she attempted to redeem the prescription at a Safeway pharmacy, she was told it had not been received. This lack of clarity and accessibility leaves many pregnant women feeling frustrated and uncertain about their options.
The American Pharmacists Association released a statement expressing concern that recent updates to COVID-19 vaccination recommendations “do not appear to be based on the scientific evidence provided over the past few years.” The abrupt changes have raised alarms among healthcare providers, who fear that the integrity of the vaccination process has been compromised. Dr. Steven J. Fleischman, president of the American College of Obstetricians and Gynecologists, warned that these changes may lead to a deterioration of vaccine confidence among pregnant women.
Health professionals are particularly concerned about the long-term risks associated with COVID-19 for both mothers and infants. Studies have indicated that infants born to mothers who had COVID-19 during pregnancy face heightened risks of stillbirth, respiratory distress, and low birth weight. “Vaccinating a mom leads to the protection of the baby when they don’t have their own immune response,” said Dr. John Lynch, an associate medical director at Harborview Medical Center.
As the conversation around COVID-19 vaccination evolves, it is essential for pregnant women to remain informed and supported by their healthcare providers to ensure their safety and the health of their infants.