A groundbreaking innovation in ophthalmology has emerged with the introduction of the PRIMA system, a tiny chip implanted into the eyes of individuals suffering from irreversible age-related macular degeneration (AMD). This remarkable advancement has successfully restored central vision in a significant number of patients, marking a pivotal moment in the quest for treatments for vision loss. The system was rigorously tested across 17 hospitals in Europe, yielding astonishing results: 26 out of 32 patients who used the implant for 12 months reported improvements in their central vision, with many even regaining the ability to read.
Age-related macular degeneration is a progressive and irreversible condition affecting millions globally. It primarily targets the macula, the part of the retina responsible for high-resolution central vision. As the macula deteriorates, individuals experience patches of blindness in their central vision, while their peripheral vision remains largely intact. This loss can be devastating for those affected, significantly impairing their quality of life. The PRIMA system, developed by Daniel Palanker, an ophthalmologist at Stanford University, has the potential to change the lives of many suffering from this debilitating condition.
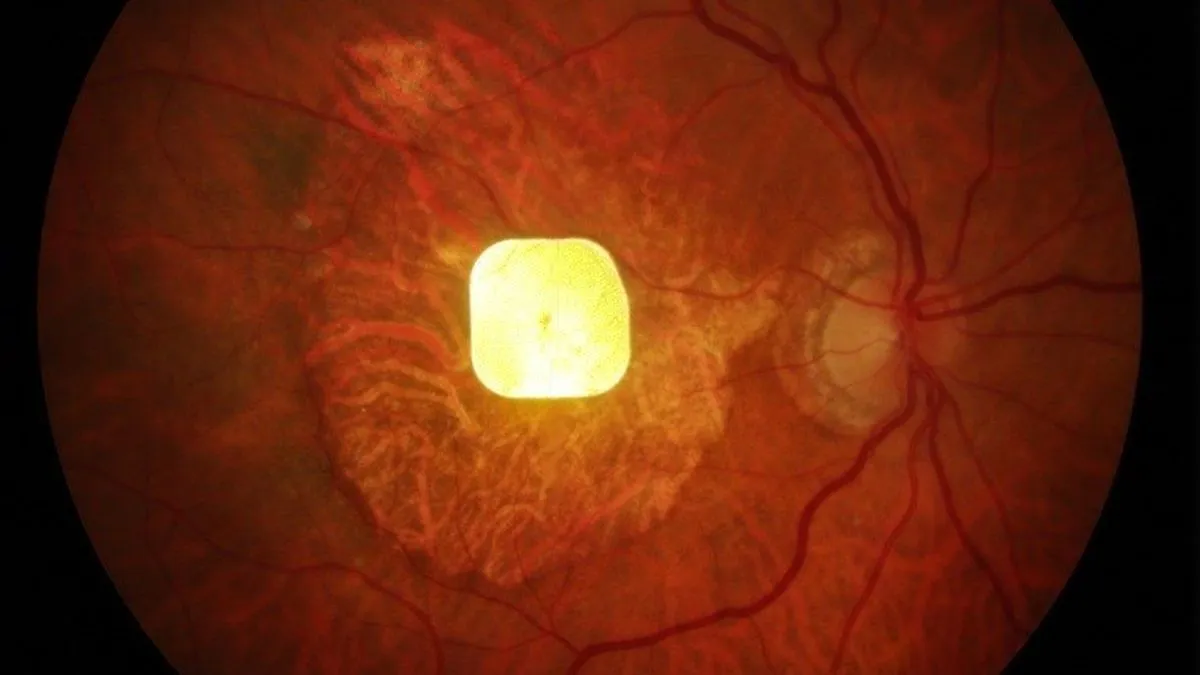
The PRIMA system consists of two main components: a tiny wireless silicon sensor and a pair of specially designed glasses. The implant, measuring just 2x2 millimeters and thinner than a human hair, features 378 photovoltaic pixels. It is positioned behind the retina, precisely where cellular atrophy occurs. The glasses, connected to a pocket processor, capture images and convert them into near-infrared light, transmitting them to the implant. This technology is crucial as near-infrared light, operating near the 880-nanometer wavelength, is invisible to the human eye, ensuring that it does not interfere with any remaining peripheral vision. The implant then translates these infrared signals into electrical impulses, mimicking the natural way the eye converts light into visual information.
After extensive clinical testing, the researchers conducted a trial involving 38 patients across five European countries. Over a 12-month period, patients underwent multiple assessments to measure their vision improvement. Initially, patients spent several months acclimating to the PRIMA system, learning to utilize its features such as zooming in on text and interpreting electrical patterns as visual shapes. Remarkably, 81% of the participants experienced significant improvements in their vision, with some achieving nearly 20/420 vision, the resolution limit of the system.
One participant, Sheila Irvine, described her experience prior to receiving the implant as having "two black discs in my eyes," making her passionate about regaining her ability to read. After the procedure, she expressed her excitement at seeing letters again, emphasizing the challenge of relearning how to read. While the PRIMA system has shown promise, it is important to note that 19 participants experienced known complications associated with eye surgery; however, these were mostly resolved quickly, and peripheral vision remained unaffected.
Currently, the PRIMA system operates only in black-and-white, but researchers are actively working on developing a grayscale version to enhance functionality. The ability to recognize faces is high on the list of patient desires, necessitating advancements in resolution. The next generation of the chip, featuring smaller pixels, aims to provide better resolution and be paired with sleeker glasses. This pioneering work in vision restoration not only represents a significant leap forward but also opens new avenues for enhancing the lives of millions affected by age-related macular degeneration.