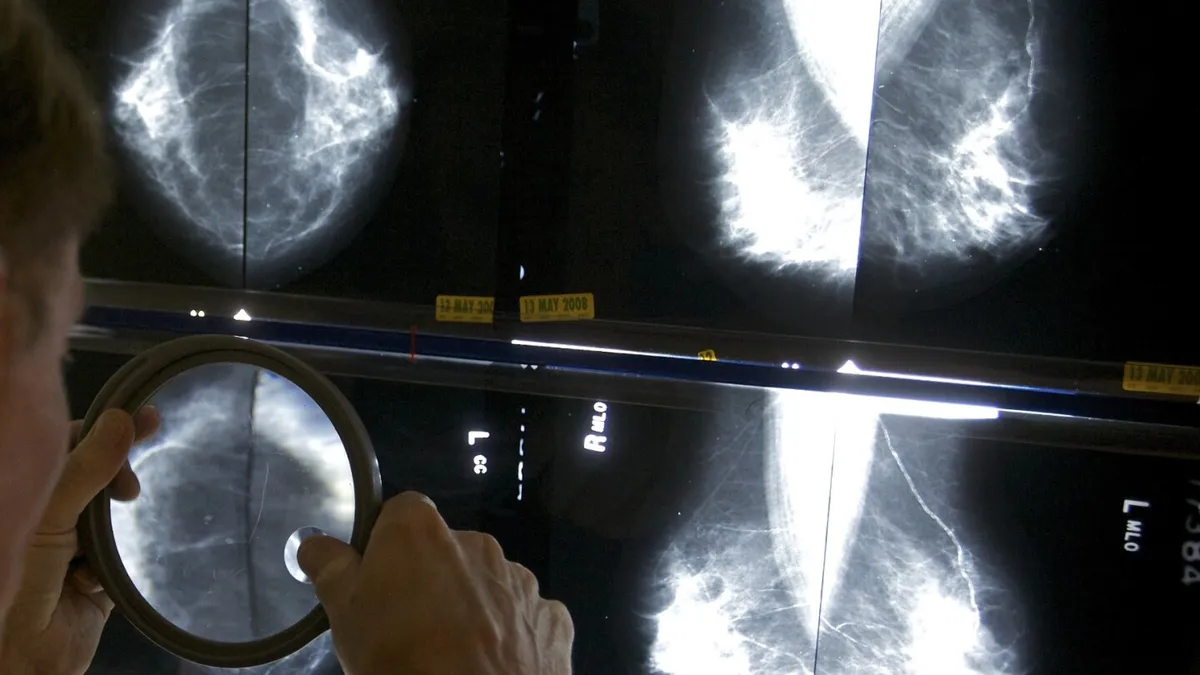
In 2020, many Americans were compelled to postpone crucial cancer screenings such as colonoscopies, mammograms, and lung scans due to the overwhelming effects of the COVID-19 pandemic on healthcare facilities. As hospitals prioritized COVID-19 patients, routine cancer screenings faced significant delays. However, recent analyses suggest that this postponement has not drastically impacted cancer statistics, at least not in the short term.
A new report published in the journal Cancer provides the most comprehensive examination to date regarding the pandemic's influence on U.S. cancer data. According to the findings, cancer death rates continue to decline, and there have not been significant increases in late-stage diagnoses. Lead author Recinda Sherman from the North American Association of Central Cancer Registries expressed reassurance, stating, “So far, we haven’t seen an excess of late-stage diagnoses,” indicating that the pandemic is unlikely to lead to higher cancer mortality rates.
Initially, in 2020, there was a noticeable uptick in the number of late-stage cancer diagnoses, which are typically more challenging to treat. However, by 2021, these concerning trends reverted to levels similar to those observed before the pandemic for most cancer types. This finding is crucial as it suggests that the healthcare system was able to recover and return to its routine operations relatively quickly.
In terms of new cancer cases, there was a decline in 2020, but by 2021, the numbers returned to pre-pandemic levels. Interestingly, the extent of the decline in new cancer diagnoses was consistent across various states, regardless of differences in COVID-19 policy restrictions. The researchers concluded that local hospital policies and human behavior had a more significant impact on cancer diagnosis rates than the broader state policies.
While there was a minor increase in late-stage diagnoses for cervical cancer and prostate cancer in 2021, the changes were not substantial. It is important to note that the data analyzed only extends through 2021, and as such, it does not provide a complete picture of the ongoing situation. Sherman remarked, “We didn’t see any notable shifts,” reinforcing the idea that individuals with aggressive cancer types were likely diagnosed in a timely manner.
This significant report is the result of collaboration between the North American Association of Central Cancer Registries, the National Cancer Institute, the Centers for Disease Control and Prevention, and the American Cancer Society. The findings aim to provide a clearer understanding of the implications of the pandemic on cancer diagnoses and treatment.
In conclusion, while the COVID-19 pandemic certainly disrupted the routine of cancer screenings, the subsequent recovery in diagnosis rates and the stability in cancer death rates offer a hopeful perspective for future cancer care. Continued monitoring and research will be essential in ensuring that all patients receive timely diagnoses and effective treatment.