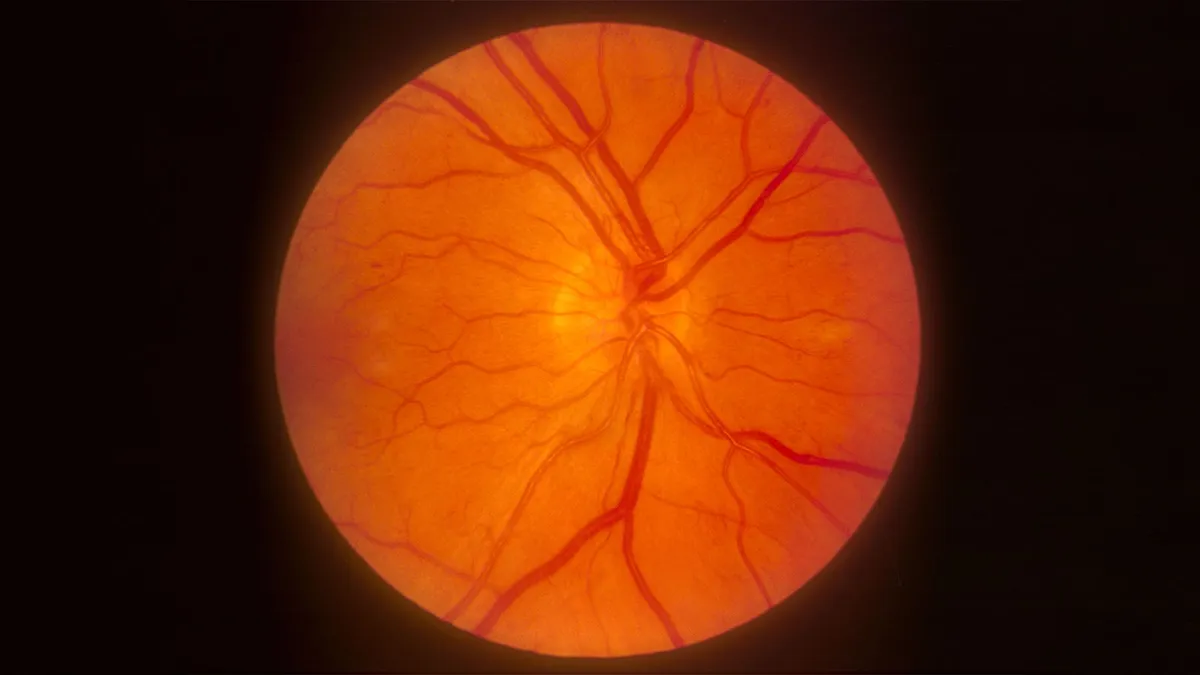
The recent findings from a large retrospective study have raised important questions regarding the use of GLP-1 receptor agonists in patients with diabetes. Although these medications are known for their effectiveness in managing blood sugar levels, the study indicates a slight yet significant increase in the risk of new-onset diabetic retinopathy (DR) among users. However, the study also found that patients using these drugs have a lower risk of developing vision-threatening complications.
Conducted by Dr. Sarju Ganatra and colleagues at Beth Israel Lahey Health in Burlington, Massachusetts, the study utilized a propensity-matched comparison to analyze the incidence of new diabetic retinopathy among patients taking GLP-1 receptor agonists. The results revealed a 7% higher incidence of new DR in this group compared to non-users. Interestingly, there was no significant difference in the risk of ischemic optic neuropathy between both groups.
In a subgroup of patients already diagnosed with DR, the use of GLP-1 drugs did not correlate with an increased risk of progression to proliferative retinopathy or diabetic macular edema (DME). The authors emphasized the importance of regular screening and monitoring for ophthalmic complications in patients with type 2 diabetes treated with GLP-1 agonists, irrespective of their baseline DR status.
The study reported that while the use of GLP-1 receptor agonists was linked to a modest increase in the rate of incident DR (a 0.2% increase over two years), the absolute number of new diagnoses remained relatively low at just 2.7%. This figure is likely below the expected annual incidence for U.S. patients with type 2 diabetes. Moreover, the use of these medications was associated with a significant 24.2% reduction in the risk of vision loss leading to blindness, with a 30.2% reduction noted in patients with pre-existing DR.
A separate but concurrent study indicated a slightly increased risk of non-arteritic ischemic optic neuropathy (NAION) in patients treated with the GLP-1 drugs semaglutide (Ozempic) or tirzepatide (Mounjaro). While the overall incidence of optic nerve disorders was low, the findings underscore the necessity for close monitoring of these conditions. The authors called for vigilance, especially in patients with pre-existing optic-disc crowding who are beginning treatment with these drugs.
Both studies together emphasize the association between incretin receptor agonists (IRAs) and eye health outcomes in diabetes patients, particularly concerning DR and NAION. This aligns with the European Medicines Agency's recent classification of NAION as a rare adverse reaction for patients using semaglutide. Despite their transformative impact on obesity and diabetes management, healthcare providers must remain cautious due to the accumulating, albeit rare, reports of NAION.
Patients starting on semaglutide or tirzepatide should be counseled about the potential, albeit rare, risk of NAION. Furthermore, individuals with DR should receive close ophthalmic monitoring, especially when initiating or intensifying therapy with IRAs. The authors suggest that a slower titration to avoid rapid glycemic fluctuations may warrant formal evaluation to enhance patient safety.
Interestingly, these studies did not include patients treated with SGLT2 inhibitors, such as empagliflozin (Jardiance) and dapagliflozin (Farxiga). Previous analyses indicate a lower incidence of sight-threatening DR when compared to other anti-diabetes treatments, including GLP-1 receptor agonists. It is noteworthy that these analyses did not find an increased risk of DR in patients treated with GLP-1 medications, which was a concern in earlier pivotal trials of semaglutide.
One of the retrospective cohort studies highlighted an increased risk of DR in patients receiving GLP-1 agonists alongside SGLT2 drugs for obesity and heart failure. However, a recent meta-analysis of 61 randomized trials indicated no significant differences among various anti-diabetic medications regarding the risk of developing DR.
In order to address limitations in previous research, Ganatra and colleagues conducted a thorough retrospective cohort analysis using data from the TriNetX database, spanning January 2015 to September 2022. They focused on adults with type 2 diabetes and an HbA1c ≥6.5%, classifying patients into a cohort with at least two prescriptions for a GLP-1 agonist and a control group. The follow-up period lasted two years, with primary endpoints centered around the association between GLP-1 medications and the risk of new DR, NAION, or sight-threatening complications.
The propensity-matched analysis included 185,066 patients, evenly split between the GLP-1 and control groups. The results indicated a hazard ratio of 1.07 for the risk of DR (95% CI 1.03-1.11), while the hazard ratio for NAION was 1.26, which did not achieve statistical significance. In a subgroup analysis involving 32,695 patients with existing DR, the use of GLP-1 agonists showed no significant association with DR progression.
A separate analysis by Xu and colleagues specifically examined the risk of optic nerve or visual pathway disorders associated with semaglutide or tirzepatide. Utilizing a national multicenter database of electronic health records, the study included 159,398 patients, half of whom were treated with the two GLP-1 drugs. The results indicated that there were 35 new cases of NAION among patients treated with semaglutide or tirzepatide, compared to 19 cases in the matched cohort, resulting in a hazard ratio of 1.76 (95% CI 1.01-3.07).
Overall, the findings from this comprehensive analysis highlight the need for ongoing vigilance and monitoring in patients with diabetes who are prescribed GLP-1 receptor agonists. As the landscape of diabetes treatment evolves, understanding the impact of these medications on eye health remains crucial for optimizing patient outcomes.