Globally, measles is experiencing a significant resurgence, particularly in regions such as the U.S., Canada, Mexico, South America, and various parts of Europe. As of 2025, North and South America reported a staggering increase in measles cases, with 11 times more infections than the same period last year. In Europe, the rates of measles have reached their highest levels in 25 years, raising alarms among health authorities.
In the United States, health authorities have confirmed 935 cases of measles across 30 states as of May 2, 2025. This figure marks a dramatic rise compared to the 285 cases reported in 2024. A particularly large outbreak has been reported in Canada, with over 1,000 cases documented. To understand the implications of these rising numbers, The Conversation reached out to Rebecca Schein, a specialist in pediatric infectious diseases.
Historically, from 2000 to 2010, the U.S. saw fewer than 100 measles cases annually. However, since 2010, isolated outbreaks have occurred, primarily in unvaccinated communities, leading to roughly 200 to 300 cases each year. The most significant outbreak in the U.S. prior to the recent surge was in 2019, with 1,274 cases predominantly in the New York City metropolitan area and parts of New Jersey.
During the COVID-19 pandemic from 2020 to 2023, measles cases fell considerably. However, in 2024, cases returned to pre-pandemic levels. Currently, the ongoing epidemic in Texas is a significant contributor to the U.S. measles figures, with 702 confirmed cases reported as of May 6, 2025. This outbreak has resulted in 91 hospitalizations and, tragically, three deaths, including two children.
Canada has reported a total of 1,177 cases as of April 19, 2025, with 951 linked to an outbreak that began in New Brunswick in October 2024 and spread across seven provinces. In stark contrast, only 12 cases were reported in Canada throughout 2023. Meanwhile, Mexico has confirmed 421 measles cases as of April 18, with an additional 384 cases still under investigation. South America is also witnessing smaller outbreaks, with Belize reporting its first two cases since 1991, Brazil documenting five cases, and Argentina confirming 21 cases in the capital city of Buenos Aires.
In Europe, the situation is equally concerning, with measles cases increasing tenfold to 35,212 in 2024, according to the European Centre for Disease Prevention and Control. The alarming rise in cases underscores the critical need for enhanced vaccination efforts across the continent.
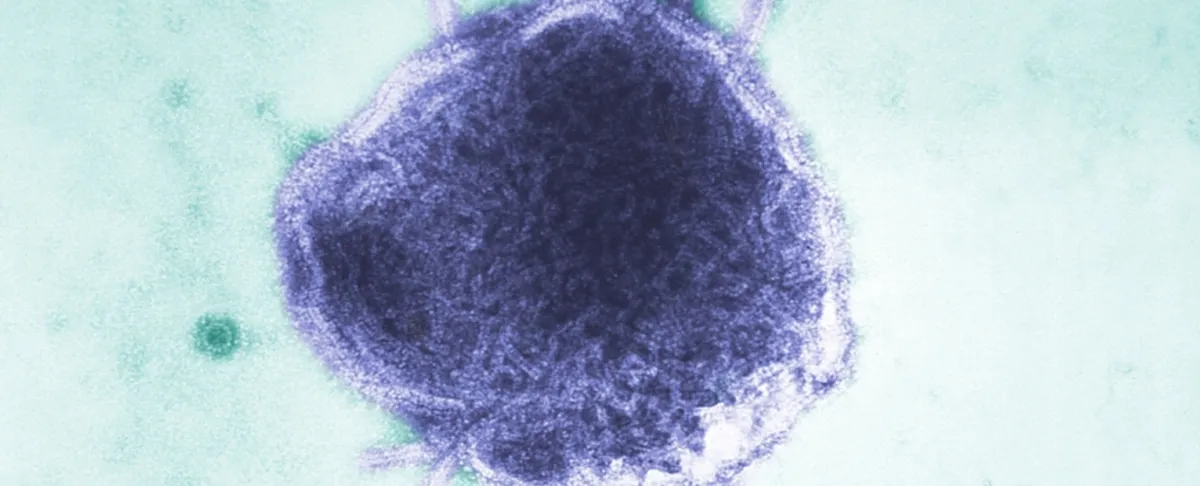
Measles is one of the most contagious diseases known. One infected individual can spread the virus to 12 to 18 others. This high transmissibility, referred to as the R0 value, is significantly higher than that of other diseases like the flu or COVID-19. In 1912, measles was designated as a nationally reportable disease in the U.S., with millions of cases and thousands of deaths annually. The introduction of a measles vaccine in 1963 led to a dramatic decline in cases, and by the year 2000, the Centers for Disease Control and Prevention declared that measles had been eliminated in the U.S.
The resurgence of measles is particularly alarming because the virus is not treatable with antibiotics, unlike bacterial infections. Vaccination is the most effective means of preventing infection. The measles vaccine typically requires two doses for optimal protection. For herd immunity, approximately 95% of the population needs to be vaccinated to effectively safeguard the community. Unfortunately, global vaccination rates have been declining over the past two decades, exacerbated by the COVID-19 pandemic, which limited access to medical care.
Public health officials classify endemic infections as those consistently present within a region. An outbreak occurs when cases exceed normal levels, while an epidemic spreads beyond local boundaries. The current measles outbreak in Texas began in January 2025 and escalated rapidly to epidemic levels, affecting 29 counties with 702 confirmed cases by May 6. A 2022 computer model study predicted that if vaccination rates do not improve, approximately 15 million U.S. children could remain vulnerable to measles over the next five years.
To reverse the trend of rising measles cases, public health initiatives must focus on increasing community vaccination rates. A recent study indicated that boosting vaccination rates by just 5% could reduce the projected rise in cases to between 3,000 and 19,000 over the next 25 years. Another model emphasized the importance of early intervention during outbreaks, suggesting that maintaining an 85% vaccination rate could effectively contain the spread of measles. Achieving this will require accessible vaccination programs and restoring public trust in the measles vaccine.
Rebecca Schein, an Assistant Professor of Infectious Disease Pediatrics at Michigan State University, emphasizes the urgent need for public awareness and action to combat the rising trend of measles infections.